Introduction to the Nobel Prize in Medicine
The Nobel Prize in Medicine, established by the will of Alfred Nobel in 1895, stands as one of the most prestigious awards in the field of medical science. This accolade is awarded annually to individuals or groups that have made significant contributions to the understanding of life sciences and advancements in medical practice. It aims to recognize exceptional work that not only enhances our knowledge but also has the potential to improve human health and welfare on a global scale. Throughout its history, the prize has highlighted innovative research and breakthroughs that have transformed our understanding of life processes and disease mechanisms.
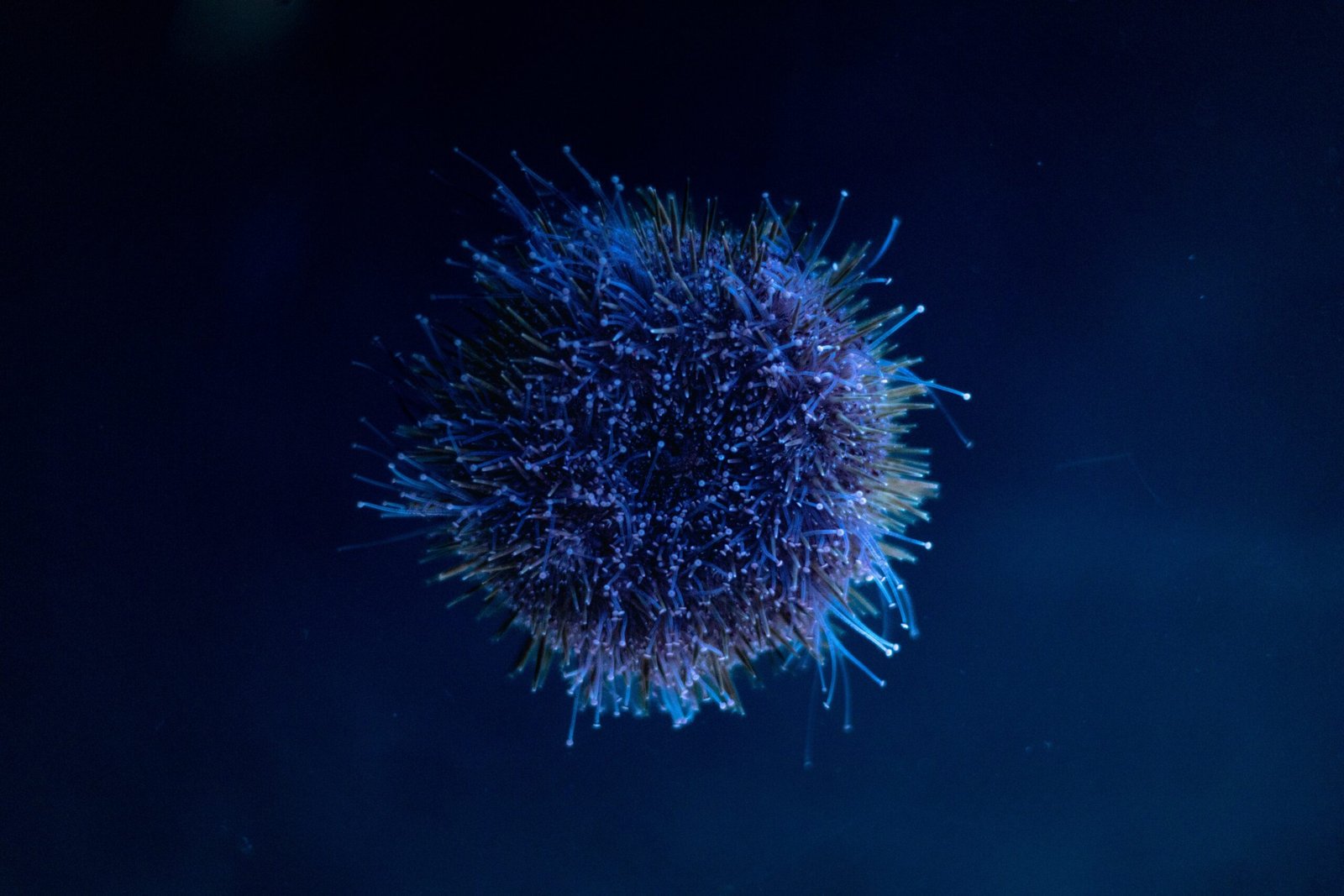
One of the pivotal areas of medical research that has garnered attention over the years is the immune system, a complex network that plays a crucial role in defending the body against pathogens. The immune system’s function is essential for maintaining health, as it distinguishes between the body’s own cells and foreign entities, enabling a robust response to infections and diseases. Consequently, the ongoing exploration into how the immune system operates has led to groundbreaking discoveries that pave the way for novel treatments and therapies, particularly in the realms of oncology and infectious diseases.
The 2025 Nobel Prize in Medicine highlights such groundbreaking discoveries related to the immune system. It underscores the vital importance of immunology in the context of contemporary medical challenges. By drawing attention to this field, the award continues to inspire ongoing research and encourages future investigations aimed at enhancing our understanding of immune responses and their implications for health and disease management. The contributions of the 2023 laureates not only illuminate the past advancements but also shape the future trajectory of medical science, reinforcing the critical relationship between immunology and global health.
The Pioneering Work of Mary E. Brunkow, Fred Ramsdell, and Dr. Shimon Sakaguchi
The contributions of Mary E. Brunkow, Fred Ramsdell, and Dr. Shimon Sakaguchi have significantly advanced our understanding of the immune system, particularly in relation to peripheral immune tolerance and regulatory T cells. Each scientist’s individual research has played a critical role in piecing together the intricate puzzle of immune system regulation.
Mary E. Brunkow’s research has primarily focused on the identification and characterization of regulatory T cells (Tregs). Her pioneering work provided insight into the mechanisms by which Tregs maintain immune homeostasis and prevent autoimmune diseases. Brunkow’s studies revealed that Tregs play an essential role in controlling immune responses to self-antigens, thus safeguarding the body from inappropriate immune responses. Through innovative experimental designs, Brunkow effectively demonstrated how the dysfunction of Tregs can lead to severe immunological complications, contributing to a broader understanding of immune tolerance.
Fred Ramsdell has been instrumental in elucidating the role of specific markers and signaling pathways that govern Treg function. His groundbreaking findings, particularly concerning the marker CD28, have helped clarify the interplay between Tregs and conventional T cells. Ramsdell’s research illuminated how effective communication among T cells is paramount for maintaining balance within the immune system. By exploring the biochemical signals that influence Treg activity, Ramsdell’s contributions have paved the way for therapeutic approaches targeting T cell responses in autoimmune disorders and other immune-related diseases.
Dr. Shimon Sakaguchi’s influential work has encompassed the functional dynamics of Tregs and their contribution to peripheral tolerance. Through his extensive research, Sakaguchi has established the critical nature of Tregs in preventing excessive immune reactions and fostering tolerance in various contexts, including organ transplantation and tumor immunity. His dedication to uncovering the basic principles that govern Treg biology has not only deepened our comprehension of immune functionality but also strengthened the foundational understanding necessary for developing novel therapeutic strategies to manipulate immune responses.
The intertwined contributions of these three eminent scientists have collectively shaped contemporary perspectives on immune system regulation. As we celebrate their groundbreaking work, it is evident that their discoveries will have lasting implications for the fields of immunology and therapeutic interventions.
Implications of Their Discoveries on Autoimmune Diseases
The groundbreaking discoveries recognized by the Nobel Prize in Medicine 2023 spotlight the critical role of regulatory T cells and peripheral immune tolerance in modulating the immune response. This understanding has significant implications for the treatment and management of autoimmune diseases, such as type 1 diabetes, rheumatoid arthritis, and lupus. Autoimmune diseases occur when the immune system erroneously attacks the body’s tissues, leading to varied and often debilitating outcomes for patients.
Regulatory T cells are essential in maintaining homeostasis within the immune system. Their primary function is to curtail excessive immune responses, preventing the immune system from mistakenly targeting healthy cells. Insights gained from recent research reveal that enhancing the functionality or population of these regulatory T cells could be pivotal in treating autoimmune disorders. For example, in type 1 diabetes, where the immune system destroys insulin-producing cells in the pancreas, therapies aimed at promoting regulatory T cell activity could halt or even reverse disease progression.
Moreover, understanding peripheral immune tolerance can lead to novel therapeutic approaches. Peripheral immune tolerance refers to the immune system’s ability to recognize and tolerate self-antigens without mounting a harmful response. Scientists are investigating ways to manipulate this tolerance to create effective treatments. For rheumatoid arthritis and lupus, therapeutic strategies that enhance this tolerance might prevent the chronic inflammation and tissue damage associated with these diseases.
The significance of these discoveries cannot be overstated, particularly for patients enduring the challenges posed by autoimmune diseases. By translating scientific findings into practical treatments, there is potential for improved quality of life and reduced disease burden. This research serves as a beacon of hope, paving the way for future therapies that could change the landscape of autoimmune disease management.
Future Directions: Applications in Medicine and Research
The groundbreaking discoveries honored with the Nobel Prize in Medicine 2023 have far-reaching implications for various fields within the medical landscape. Researchers and clinicians alike are now exploring how insights into immune system function can translate into tangible benefits for patient care. One significant area of focus is organ transplantation. The understanding of immune response modulation may lead to better strategies for improving organ compatibility and reducing the risk of rejection. Ongoing research investigates innovative immunosuppressive protocols derived from recent findings, aiming to enhance patient outcomes while minimizing side effects.
In addition to advancements in transplantation, the discoveries have heightened interest in cancer therapies. The immune system plays a pivotal role in recognizing and attacking cancer cells. Therefore, enhancing the immune response through targeted therapies heralds new possibilities in oncology. Scientists are currently developing methods that harness the immune system’s natural aptitude for identifying malignancies, with ongoing clinical trials assessing the effectiveness of these novel treatments. These approaches signify a shift towards personalized medicine, where therapies are tailored based on an individual’s unique immune profile.
Furthermore, the work awarded this year fosters progress in addressing autoimmune diseases. Conditions such as rheumatoid arthritis and lupus arise from immune system malfunctions. Current studies are concentrating on identifying specific immune pathways that contribute to these disorders, with the aim of developing effective therapeutics that better regulate immune activity without compromising the body’s ability to fend off pathogens. The potential for breakthroughs in this area is substantial, as targeted treatments can facilitate improved quality of life for millions affected by these chronic diseases.
Overall, the contributions of these esteemed scientists underscore the importance of continued research in immunology. Their findings not only lay the groundwork for future innovations but also reinforce the need for interdisciplinary collaboration moving forward. As we delve deeper into the complexities of the immune system, the potential for transformative medical advancements continues to grow.